By Dr Fiona McMillan
New research from the University of Queensland Diamantina Institute reveals how an existing treatment for rheumatoid arthritis could be used to prevent the spread of osteosarcoma tumours.
Osteosarcoma (OS) accounts for 56% of all malignant bone cancers and 6% of childhood and adolescent cancers. The prognosis depends heavily on whether or not the cancer has spread at the time of diagnosis. If the tumour is still localised at the bone, the 5 year survival is around 70% with treatment. But once the cancer has begun to spread, or ‘metastasise’, the 5 year survival drops to around 20%. These patients don’t respond well to standard treatment.
We still know very little about the cellular and molecular changes that cause an OS tumour to spread and become life threatening. UQDI researcher Dr Liliana Endo Munoz explains that to understand this, we need to take a closer look at the diversity among the different cancer cells within a tumour.
“Any OS tumour is very heterogeneous and we know there are cells that are metastatic and cells that are non-metastatic and everything in between,” she explains.
“There is quite a lot of genetic diversity among tumour cells within the same tumour. We also know that in a number of other cancers, this genetic variation contributes to some cells becoming resistant to therapy or acquiring the ability to spread.”
Dr Endo Munoz wanted to find out how much the potential for metastasis varied between cells in a single OS tumour, and to then determine which genes contribute to those differences.
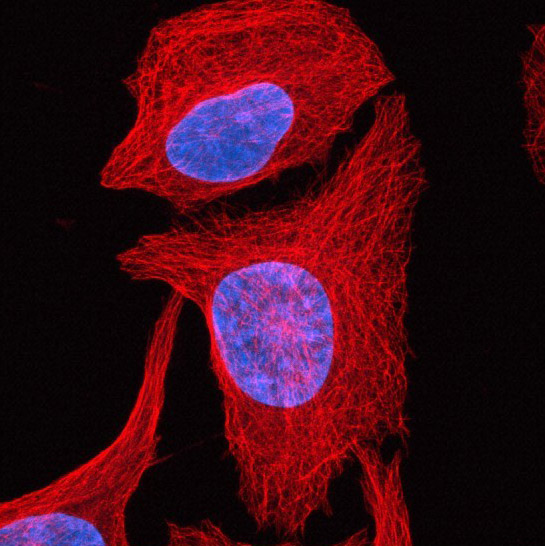
She and her colleagues isolated several single cells from a type of OS tumour known to easily spread to the lungs. They then grew a separate population of cells from each of these individual cells and examined how well each cell population was able to spread.
“What we found is that they are all metastatic, but with different abilities.”
Four of the cell populations were less metastatic than the original ‘parent’ tumour, but two of the cell populations were more metastatic. The question then, is what is the difference between the cells that are highly metastatic and the cells that are poorly metastatic? After all, they all came from the same original tumour.
Dr Endo Munoz looked at the differences in gene expression, which told them which genes were turned on or off and by how much. From this they identified twenty genes that were highly upregulated in highly metastatic cells. In other words, OS cells that could spread easily were making much higher levels of the protein products of these twenty genes.
Endo Munoz and her colleagues then sought to take a closer look how these twenty genes were behaving in human OS patients, so they analysed biopsies from a range of metastatic and non-metastatic OS tumours.
From this comparison, they were able to substantially narrow down the list. The most significant result was the finding that in 30% of the biopsies, the gene that codes for a protein called Thioredoxin Reductase 2 (TXNRD2) was highly upregulated. TXNRD2 is normally known for its critical role in the function of a cell’s powerhouse, the mitochondria. This finding raised two compelling questions: is over-production of TXNRD2 required for an OS tumour to spread? And if so, would blocking TXNRD2 prevent an OS tumour from spreading?
It turns out that TXNRD2 is the target of an existing drug, Auranofin, which was used for many years in the treatment of rheumatoid arthritis. Dr Endo Munoz and her colleagues tested Auranofin on human OS tumour cells and found that it indeed inhibits TXNRD2.
They then tested the effect of Auranofin on mice with OS and found that the drug significantly inhibits the spread of OS to the lungs. While the primary tumour appears to be resistant to Auranofin, perhaps due in part to a protective effect of the local environment, as soon as tumour cells begin to break off and metastasise, they become highly vulnerable to the drug. The findings were published in the journal Oncotarget.
Dr Endo Munoz and her fellow researchers have recently commenced pre-clinical testing of Auranofin on dogs with OS. There was a dual purpose in this: not only is it an important stepping stone to human trials, but OS is also a major problem for dogs. In fact, dogs develop OS at a much higher rate than humans do. More than 8000 cases of canine OS are reported every year by veterinarians in the US. While the disease tends to occur mostly in adolescence in humans, it more often affects dogs as they get older (6 years and up), but other than this distinction the disease progression is remarkably similar in both species. Moreover, just as in humans, at the point of diagnosis some OS tumours have metastasised and some haven’t, and it’s important to keep the non-metastasised cancers from spreading.
It’s too early for a concrete result, says Dr Endo Munoz, explaining that the dog trial will need to run for at least another year. However she says that she is encouraged by the early data, which is showing promise. If Auranofin does indeed prove to be effective at preventing OS from spreading, she envisions that it could be administered as soon as a patient is diagnosed and continued in conjunction with standard treatments, keeping the cancer in one place where it can be targeted, and ideally, eliminated.
Media: Kate Templeman, k.templeman@uq.edu.au +61 7 3443 7027, +61 (0)409 916 801