 University of Queensland researchers have used a protein inhibitor to clear the notorious food-borne pathogen Listeria monocytogenes from immune cells.
University of Queensland researchers have used a protein inhibitor to clear the notorious food-borne pathogen Listeria monocytogenes from immune cells.
The UQ Diamantina Institute’s Professor Antje Blumenthal said production of bacterial virulence proteins that enable Listeria to multiply in immune cells are controlled by a bacterial master regulator protein, known as PrfA.
“Once ingested, Listeria can hide from the immune system and multiply inside immune cells,” said Professor Blumenthal.
“Instead of killing the bacteria, the immune cells are killed by Listeria growing inside them.
“Our study showed the bacteria could be cleared with a small drug-like inhibitor that targets PrfA, helping immune cells survive infection,” said Professor Blumenthal.
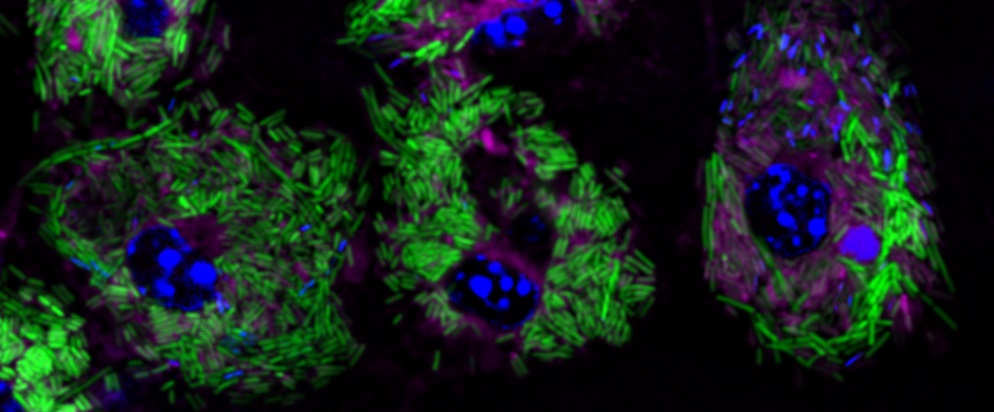
“We tracked what happens to Listeria when PrfA is inhibited over several days using molecular imaging and infection studies.”
Until now, understanding how PrfA makes Listeria virulent has been largely based on bacteria being engineered to lack the PrfA protein or carry a mutated version of PrfA.
Professor Blumenthal said Listeria bacteria can survive in fridges and cause major outbreaks through contaminated foods such as fresh produce, dairy products, and meats.
“Listeria infection can be dangerous and even deadly for the immunocompromised.
“It is also a major health concern during pregnancy and infection can lead to miscarriage, stillbirth, or premature birth,” said Professor Blumenthal.
“Our discovery, together with recent milestones in understanding the molecular and structural requirements for PrfA functions, may guide design of PrfA inhibitors that can be developed into drugs that help treat Listeria infection.
“This could add new options for treating Listeria infections and improve health outcomes for patients with complications arising from listeriosis,” she said.
“Our findings could also guide design of inhibitors against other PrfA-like proteins that are found in different bacteria.”
The study is published in the journal PLOS Pathogens (DOI: 10.1371/journal.ppat.1010166).
It was conducted in collaboration with Umeå University, Sweden; UQ School of Chemistry and Molecular Biosciences; Australian Infectious Diseases Research Centre; Institute for Molecular Bioscience; Mater Research Institute; Telethon Kids Institute, University of Western Australia; Monash University; University of Melbourne at the Peter Doherty Institute for Infection and Immunity and Hudson Institute of Medical Research.